Migraine: The Third Leading Cause of Disability Worldwide
Migraine ranks third among causes of disability worldwide according to the Global Burden of Disease Study (GBD, Lancet, 2018). It affects approximately 1 billion people: 18% of women and 6% of men. Despite its prevalence, migraine remains one of the most underdiagnosed and inadequately treated neurological conditions.
Migraine vs Cluster Headache vs Tension-Type Headache
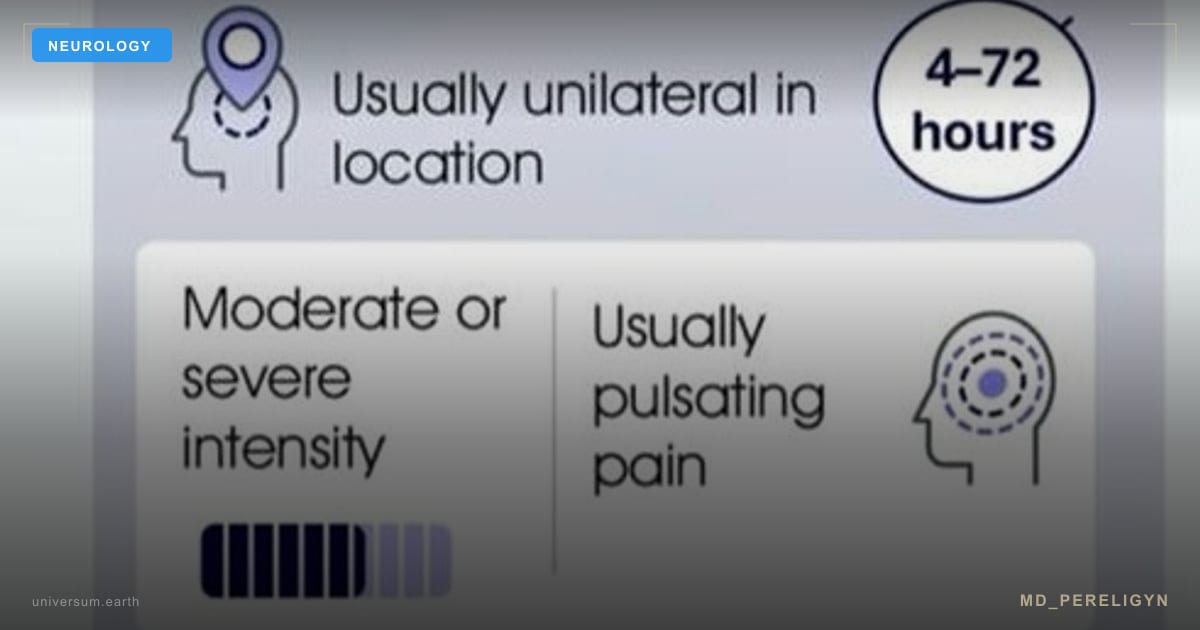
Migraine: - Unilateral (60% of cases), pulsating quality - Moderate-to-severe intensity (4-10 on VAS) - Duration: 4-72 hours - Associated features: nausea/vomiting, photophobia, phonophobia - Aggravated by physical activity - Aura precedes attack in 25-30%: visual phenomena, paresthesias, speech disturbance
Cluster headache: - Strictly unilateral, periorbital, "ice pick" quality - Maximum intensity (10/10, "suicide headache") - Duration: 15-180 minutes - Autonomic features: lacrimation, nasal congestion, miosis, ptosis - Cyclic pattern: cluster periods 4-12 weeks, remissions months to years
Tension-type headache: - Bilateral, pressing/tightening ("band-like") - Mild-to-moderate intensity (2-6 on VAS) - Duration: 30 minutes to 7 days - No nausea; mild photo- or phonophobia possible - Not aggravated by physical activity
Aura: Neurophysiology and Clinical Significance
Aura is transient focal neurological symptoms preceding or accompanying migraine. It results from cortical spreading depression (CSD) — a wave of neuronal excitation followed by depression propagating across the cortex at 3-5 mm/min.
Most common aura types: - Visual (90%): scintillating scotoma, zigzag lines, tunnel vision - Sensory (30%): paresthesias, numbness (typically hand to face) - Speech (10%): aphasia, dysarthria
Migraine with aura is associated with increased ischemic stroke risk (RR 2.16, meta-analysis Schurks et al., BMJ, 2009), especially in women taking COCs who smoke.
The CGRP Pathway: A Revolution in Understanding Migraine
Calcitonin gene-related peptide (CGRP) is a neuropeptide central to migraine pathophysiology. When the trigeminovascular system is activated, trigeminal sensory neurons release CGRP, causing meningeal vasodilation, neurogenic inflammation (mast cell degranulation, pro-inflammatory cytokine release), and peripheral and central sensitization.
Serum CGRP levels rise during migraine attacks and correlate with pain intensity (Goadsby et al., NEJM, 2017). This discovery spawned an entirely new drug class — anti-CGRP therapy.
Triptans: The Gold Standard for Acute Treatment
Triptans (sumatriptan, zolmitriptan, rizatriptan, eletriptan) are 5-HT1B/1D receptor agonists. They constrict meningeal vessels, inhibit CGRP release, and block pain transmission in the trigeminal nucleus. Meta-analysis by Ferrari et al. (Lancet, 2001): eletriptan and rizatriptan showed the highest efficacy.
Critically, taking a triptan within the first 30-60 minutes of an attack increases efficacy from 30% to 70%. Later use — after central sensitization (allodynia) develops — is far less effective.
Contraindications: coronary artery disease, uncontrolled hypertension, history of stroke, basilar and hemiplegic migraine.
Evidence-Based Migraine Prevention Protocol
### Magnesium (L-Threonate)
Magnesium deficiency is found in 30-50% of migraine patients. Magnesium modulates NMDA receptors, serotonin receptors, and stabilizes CSD. RCT by Peikert et al. (Cephalalgia, 1996): 600 mg magnesium daily reduced attack frequency by 41.6%. L-threonate form preferred for superior blood-brain barrier penetration. Dosage: 144 mg elemental magnesium (2,000 mg L-threonate) daily.
### Coenzyme Q10 (Ubiquinol)
CoQ10 improves mitochondrial function. Mitochondrial energy deficit is one mechanism predisposing to CSD. RCT by Sandor et al. (Neurology, 2005): CoQ10 300 mg/day reduced attack frequency by 47.6% over 3 months. Recommendation: 200-400 mg/day ubiquinol.
### Riboflavin (Vitamin B2)
Riboflavin is a cofactor in the mitochondrial electron transport chain. RCT by Schoenen et al. (Neurology, 1998): 400 mg/day reduced migraine frequency by 50% in 59% of patients. Minimum evaluation period: 3 months.
### Botulinum Toxin (Botox)
OnabotulinumtoxinA is approved for chronic migraine prevention (15 or more headache days/month, of which 8+ are migrainous). PREEMPT protocol: 155-195 units across 31-39 injection sites every 12 weeks. Dodick et al. (Headache, 2010): reduction of 8-9 headache days per month.
### Anti-CGRP Monoclonal Antibodies
Erenumab (Aimovig), fremanezumab (Ajovy), galcanezumab (Emgality) — monthly subcutaneous injections. Reduce migraine frequency by 50%+ in 50-60% of patients (Goadsby et al., NEJM, 2017). Well tolerated with minimal side effects. Indicated after failure of 2+ conventional preventive medications.
Non-Pharmacological Prevention Strategies
Regular sleep: 7-8 hours with consistent sleep-wake times (including weekends). Irregular sleep is among the top triggers. Diet: Eliminate individual triggers (alcohol, chocolate, aged cheeses, MSG, nitrites). Ketogenic diet: pilot study by Di Lorenzo et al. (European Journal of Neurology, 2015) showed 80% reduction in migraine frequency. Exercise: 30-45 minutes of aerobic activity 3-5 times weekly. Varkey et al. (Cephalalgia, 2011): regular exercise is comparable in efficacy to topiramate. Stress management: CBT, biofeedback, meditation. Most effective when combined with pharmacotherapy.
Frequently Asked Questions
How do you distinguish migraine from a dangerous headache? Red flags: sudden severe onset ("thunderclap"), new onset after age 50, progressive worsening, neurological deficits (weakness, diplopia, seizures), fever, neck stiffness. Any of these require immediate neuroimaging (MRI/CT).
Can triptans be taken daily? No. Using triptans more than 10 days/month leads to medication-overuse headache. Maximum: 2-3 days per week.
How long before prevention takes effect? Minimum 2-3 months of consistent use (magnesium, CoQ10, riboflavin). Anti-CGRP antibodies may work from the first month. Botox typically after 2-3 sessions.
Is migraine hereditary? Yes. Genetic predisposition is well established. First-degree relatives have 2-4 fold increased risk. Migraine with aura has a stronger genetic component.
Is magnesium safe during pregnancy? Magnesium citrate and glycinate are safe during pregnancy and are among the few permitted preventive options for pregnant migraineurs. Data on L-threonate in pregnancy is insufficient.
*This article is for educational purposes only and does not constitute medical advice. Always consult a qualified healthcare professional before starting any treatment.*