The Most Common Endocrine Disorder in Women
Polycystic ovary syndrome (PCOS) affects 8-13% of reproductive-age women, making it the most prevalent endocrine disorder in women (Bozdag et al., Human Reproduction Update, 2016). Up to 70% of cases remain undiagnosed. The average time from symptom onset to diagnosis exceeds 2 years, with patients seeing an average of 3 physicians before receiving the correct diagnosis.
Rotterdam Criteria: Establishing the Diagnosis
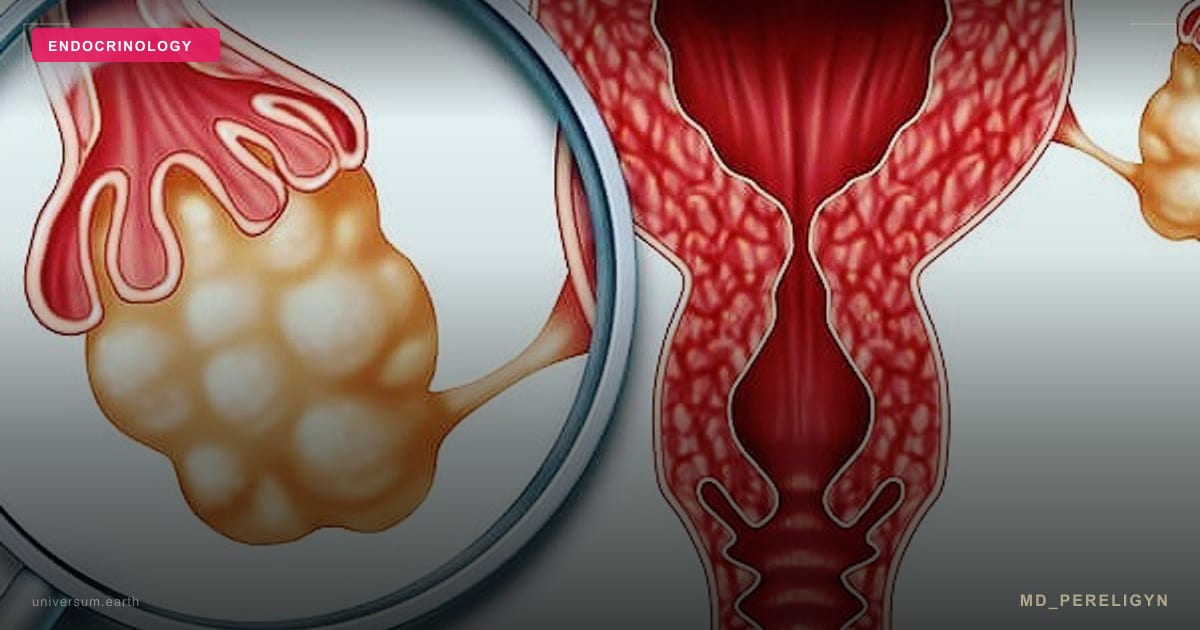
PCOS is diagnosed when at least 2 of 3 criteria are present (Rotterdam Consensus, 2003):
1. Oligo-ovulation or anovulation — irregular cycles (>35 days) or amenorrhea 2. Clinical and/or biochemical hyperandrogenism — acne, hirsutism, alopecia, elevated free testosterone or DHEA-S 3. Polycystic ovarian morphology on ultrasound — 12 or more follicles measuring 2-9 mm and/or ovarian volume >10 mL
Important: other causes of hyperandrogenism must be excluded — congenital adrenal hyperplasia (17-OH progesterone), Cushing syndrome (cortisol), prolactinoma (prolactin), hypothyroidism (TSH).
Insulin Resistance: The Root Cause in 70% of Patients
Insulin resistance is present in 70-80% of women with PCOS (both obese and lean). The mechanism: excess insulin stimulates ovarian theca cells to overproduce androgens (testosterone, androstenedione) and reduces SHBG, increasing bioavailable free testosterone.
Diagnostic workup for insulin resistance in PCOS: - Fasting insulin (>10 uIU/mL suspicious, >15 highly suggestive) - HOMA-IR index = glucose (mmol/L) x insulin (uIU/mL) / 22.5 (normal <2.0, PCOS often >3.0) - Oral glucose tolerance test (OGTT) with insulin — 0, 30, 60, 120 minutes - HbA1c — for chronic glycemia assessment
Anti-Mullerian Hormone (AMH): A PCOS Biomarker
AMH is produced by granulosa cells of preantral and small antral follicles. In PCOS, AMH is elevated 2-3 fold (>4.7 ng/mL) due to the large number of immature follicles. Dewailly et al. (Human Reproduction Update, 2014) proposed AMH as an additional diagnostic criterion.
Why Birth Control Does Not Solve the Problem
Combined oral contraceptives (COCs) are the standard first-line treatment in gynecological practice. They suppress ovarian androgens, regulate cycles, improve acne and hirsutism, and protect the endometrium.
However, COCs do NOT address insulin resistance. In fact, Diamanti-Kandarakis et al. (JCEM, 2003) showed that certain COCs worsen insulin resistance. Upon discontinuation, all symptoms return — often more severely.
Comprehensive PCOS Treatment Protocol
### 1. Inositol (Myo-inositol + D-chiro-inositol)
Myo-inositol (MI) is a second messenger in insulin signaling. MI deficiency is a key mechanism of insulin resistance in PCOS. Meta-analysis by Unfer et al. (Gynecological Endocrinology, 2017): MI 4,000 mg/day + DCI 110 mg/day (40:1 ratio) significantly reduces testosterone, improves ovulation, and lowers fasting insulin. Recommended: MI 2,000 mg + DCI 55 mg twice daily.
### 2. Metformin
An insulin sensitizer that reduces hepatic glucose production. Cochrane meta-analysis (Morley et al., 2017): metformin improves ovulation, reduces androgens, and decreases weight in PCOS. Starting dose: 500 mg, titrated to 1,500-2,000 mg/day.
### 3. Spironolactone
An aldosterone antagonist with anti-androgenic activity. Blocks androgen receptors and inhibits 5-alpha reductase. Dosage: 50-200 mg/day. Effects on acne and hirsutism appear after 3-6 months. Contraception is mandatory (teratogenic risk).
### 4. Lifestyle Management
Nutrition: Mediterranean diet with low glycemic index. Meta-analysis in Nutrients (2020): reducing dietary GI significantly decreases fasting insulin, androgens, and improves ovulation in PCOS.
Exercise: 150 minutes moderate aerobic activity plus 2 resistance training sessions per week. A 5-10% weight loss normalizes ovulation in 55-80% of overweight women with PCOS (Moran et al., Human Reproduction Update, 2011).
Supplements: - Vitamin D3: 2,000-4,000 IU/day (deficiency in 67-85% of PCOS patients) - Omega-3: 2,000 mg EPA+DHA (reduces inflammation and triglycerides) - Berberine: 500 mg three times daily (insulin sensitizer comparable to metformin) - N-acetylcysteine (NAC): 1,800 mg/day (improves ovulation and insulin sensitivity)
Frequently Asked Questions
Can you get pregnant with PCOS? Yes. Correcting insulin resistance (inositol + metformin + lifestyle) restores ovulation in most women. If needed, letrozole is the preferred ovulation induction agent (superior to clomiphene per NEJM meta-analysis, 2014).
Is PCOS permanent? PCOS is a chronic condition with genetic predisposition. However, symptoms can be controlled and minimized by addressing insulin resistance.
Should PCOS be treated if pregnancy is not planned? Yes. Untreated PCOS increases risk of type 2 diabetes (5-8 fold), cardiovascular disease, endometrial hyperplasia and cancer, depression, and metabolic syndrome.
Is inositol better than metformin? Inositol is better tolerated (fewer GI side effects), available without prescription, and comparably effective. The optimal strategy is combining both.
*This article is for educational purposes only and does not constitute medical advice. Always consult a qualified healthcare professional before starting any treatment.*